Most cases of unpleasant pain in the lumbar region and spine are associated with a disease such as osteochondrosis. It affects about 40% of men and women aged 30-40 years and about 90% of the elderly. Therefore, the earlier the disease is diagnosed, the more thoroughly the patient is examined, the more likely it is to stop the progression of osteochondrosis and to maintain activity in later life.

Determining the disease, the cause of the disease
So, what is osteochondrosis, where does it develop, what structures does it affect, what is the method of treatment? The disease affects the spine and the tissues between the vertebrae and is expressed in a violation of their shape, density, elasticity, and sometimes even integrity. As a result, the distance between the vertebrae is reduced, the spine gradually loses its stability, pinching the nerves, hernia formation may develop, which is accompanied by back pain and discomfort during movement.
If we briefly describe the nature of osteochondrosis, it is a gradual erasure of the tissues of the intervertebral discs (cartilage), leading to instability of the spine. If left untreated, degradation of ligaments and joints develops, osteophytes appear, posture is impaired, movements are accompanied by pain.
Causes of osteochondrosis of the spine:
- inactive lifestyle with a deficit of muscle load;
- spinal cord injury;
- systematic intense stress on the spine;
- heredity;
- Overweight;
- hypothermia;
- hormonal and autoimmune diseases;
- toxic poisoning;
- congenital connective tissue failure;
- psychosomatic causes (stress, depression, etc. ).
Symptoms of osteochondrosis
The disease is characterized by periods of remission and exacerbation with varying degrees of severity of symptoms. The main symptoms of spinal osteochondrosis, characteristic of the main types of disease, lumbar, cervical and thoracic:
- pain localized in a certain area of the spine;
- reflected pain syndrome associated with damage to nearby musculoskeletal tissues;
- myelopathy and radiculopathy as a result of compression of the nerve endings of the spinal cord and blood vessels.
Depending on which part of the spine is affected by the disease, the list of symptoms of osteochondrosis can vary. Namely: patients report tingling in the muscles, tingling in the limbs, other sensory disturbances, decreased strength in the arms and legs, headache and heart pain, low back pain.
The pathogenesis of osteochondrosis
Before the elastic fibrous nucleus of the intervertebral disc begins to lose elasticity and deform, a number of processes take place in the human body, including osteochondrosis:
- spasms, dystonia, inflammation;
- decreased blood circulation;
- damage to nerve cell processes.
In addition, cracks appear on the deformed ring, a protrusion of the discs develops and a hernia forms. These predisposing factors for spinal disease usually develop in childhood or adolescence and are often the result of poor posture, scoliosis, sports injuries, infectious diseases, or congenital vascular disorders.
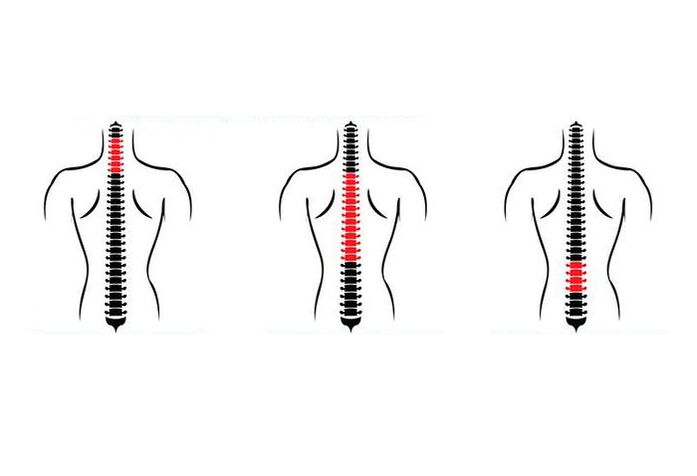
Stages of osteochondrosis
There are three stages in the development of spinal osteochondrosis:
- the first, in which the intervertebral disc begins to decrease in height, acquiring a flattened shape, loses moisture, elasticity, may protrude;
- the second develops in the absence of treatment and is manifested by a violation of the structure of the fibrous ring of the spinal disc, the appearance of cracks and the development of instability in a certain area of the spine;
- it is characterized by ruptures of the intervertebral cartilage, development of hernias, formation of bone processes of osteophytes.
The symptoms of osteochondrosis of the spine become more intense from the first to the third stage.
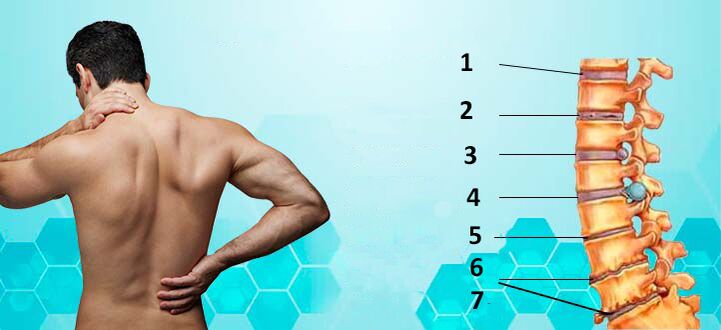
Classification of osteochondrosis
The classification of osteochondrosis is based on several features, the main of which is the area of localization. Distinguish:
- lumbar osteochondrosis;
- osteochondrosis of the cervical spine;
- thoracic osteochondrosis.
Osteochondrosis in the lumbar spine is manifested by pain in the lumbar region, which increases with turning the body, lifting weights. Pain can be given to the legs or both legs, characterized as pain. Acute syndrome is suspected hernia. In lumbar osteochondrosis often occur spasms in the muscles of the legs, flaking of the skin.
With the development of osteochondrosis of the spine in the cervical spine are affected vertebrae 1-7. The disease is accompanied by headache in the back of the head, pain in the neck, collarbones, shoulders. It is possible to crunch during the rotation of the head, tingling in the upper limbs, a feeling of a lump in the throat.
With osteochondrosis of the spine in the chest area, the patient is worried about pain in the chest, shoulders, armpits, heart. Perhaps a feeling of shortness of breath, the development of attacks of intercostal neuralgia.
Osteochondrosis in the lumbar spine is the most common, in the chest is the rarest.
Complications of osteochondrosis
If the patient has considered the treatment of osteochondrosis too late, when the symptoms of the disease are pronounced, the following complications may develop:
- intervertebral hernia;
- stroke of the spinal cord;
- kyphosis of the spine;
- protrusion;
- radiculitis;
- paralysis of the lower limbs.
In the absence of treatment, the patient begins to suffer from regular exacerbations of the condition, which are characterized by increased pain, restricted movement, a sharp deterioration in general well-being. The most serious complication of spinal osteochondrosis is injury. Therefore, in order to prevent such serious changes in the functioning of the musculoskeletal system, quality and timely treatment of osteochondrosis is necessary.

Diagnosis of osteochondrosis
A disease such as osteochondrosis is primarily a pain in the spine. But it is important to distinguish it from pain caused by problems other than intervertebral disc degeneration. To do this, doctors perform a step-by-step diagnosis, which includes:
- Taking anamnesis, which involves a conversation between a specialist and a patient to identify the exact area of localization of pain, factors that provoke deterioration of the condition. It is important to know the patient's profession, the period in which the problems with the spine began, when there was an exacerbation, what pain in the lumbar and other regions occurs, what methods of treatment the patient used.
- Physiological examinationallows you to determine the proportions of the body, the quality of movements and actions, the condition of the skin, the degree of sensitivity to pain. The doctor determines the condition of the muscle tissue, the presence of seals, swelling, etc. by palpation.
- Radiography of the spine in two planesfor visual assessment of the condition. Allows you to determine the displacement of the vertebrae, the presence of osteophytes, salt deposition.
If the collected data for prescribing treatment are insufficient or there is a suspicion of serious pathology of the spine, the patient is prescribed CT and magnetic resonance imaging, thanks to which it is possible to examine in detail the vertebrae, vessels, soft tissues, nervous processes andcreate a complete picture of the condition of the spine affected by osteochondrosis, to determine treatment tactics.
Treatment of osteochondrosis
Like any disease, osteochondrosis requires the identification of the cause that triggered its development. Reducing the severity of symptoms is not the main, but an important stage of treatment, the outcome of which depends on a number of factors. In some cases it is a complete cure, in others - the prevention of complications and injuries.
In the treatment of osteochondrosis of the spine, a group of measures is used:
- change in the patient's daily routine;
- prescribing medications to reduce symptoms;
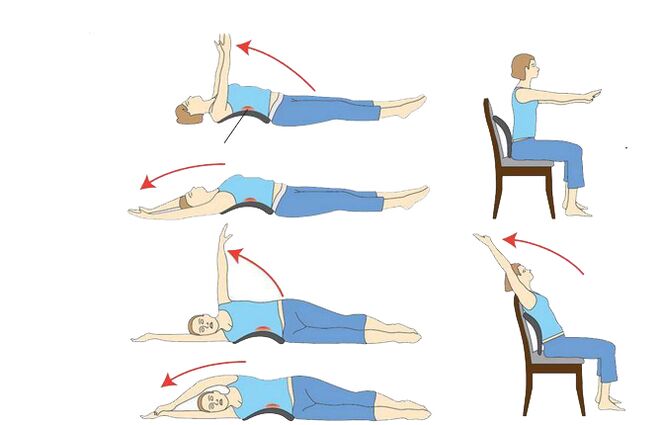
- physiotherapy procedures (massage, acupuncture, electrophoresis, exercise therapy, etc. ).
Changing the daily regimen for the treatment of osteochondrosis of the spine includes reducing the intensity of physical activity, bed rest with severe pain, exclusion of sharp turns and bends.
Drugs for the treatment of osteochondrosis of the spine
They can be divided into several groups:
- muscle relaxants for pain relief, including tablets, injectable anesthetics and anti-inflammatory injections for osteochondrosis. The homeopathic preparation normalizes the functionality of the thyroid gland, improves lymphatic drainage, has anti-inflammatory, detoxifying and immunomodulatory effects.
- non-steroidal anti-inflammatory drugs. When used in patients with osteoarthritis, it reduces the progression of inflammatory and destructive changes in the joints, improves the integrity, thickness and other characteristics of cartilage and stimulates bone regeneration.
- anti-inflammatory topical ointments and alternative transdermal patches. Such drugs have analgesic, antirheumatic, antipyretic and anti-inflammatory effects. The mechanism of action is to reduce the production of inflammatory mediators, to reduce body temperature and pain.
- chondroprotectors;
- therapeutic analgesic blockers;
- B vitamins.
Additional treatments
Of the additional agents that can be used to treat, alleviate the general condition and improve the function of the spine and intervertebral discs, the most effective are shown:
- acupuncture;
- magnetic therapy;
- professional massage and self-massage;
- physical education courses;
- manual therapy.
Prognosis, prevention
If the disease of the spine is not neglected, proceeds without serious complications, for 1, 5-2 months of competent treatment, the condition can be significantly improved and prevent the transition of the disease to a chronic form. In difficult cases, doctors recommend surgical treatment.
Prevention of spinal osteochondrosis includes:
- adherence to a proper daily routine, with a change in body position and moderate physical activity;
- regular visits to the pool;
- weight control;
- wearing comfortable shoes;
- balanced diet;
- sleeping on an orthopedic pillow and mattress;
- taking missing nutrients or preventative homeopathic remedies to boost immunity, improve overall health and eliminate dystonia.
It is necessary to undergo annual medical examinations and consult a doctor for treatment immediately after the onset of back pain.
It does not matter what kind of osteochondrosis we are talking about - lumbar, cervical or thoracic, attention to one's own health should become a good habit, especially when it comes to the basis of the entire musculoskeletal system - the spine.





































